Folliculitis after hair transplant is inflammation or infection of hair follicles at the donor or recipient scalp sites, appearing as small, red bumps or pus-filled lesions around individual hair follicles. This condition affects approximately 12.1% of hair transplant patients and typically develops within the first few weeks after follicular unit extraction (FUE) or strip harvesting (FUT) procedures.
Folliculitis after hair transplant is generally mild and resolves within 7-10 days with proper care. Understanding how to recognize, prevent, and treat this condition ensures optimal recovery and protects your hair transplant results.
Key Points
- Folliculitis appears as red bumps or pustules around transplanted hair grafts and affects about 12.1% of patients.
- Symptoms typically develop 1-3 weeks after your hair transplant and resolve within 7-10 days with proper treatment.
- Common causes include inadequate scalp hygiene, bacterial overgrowth, and delayed post-operative washing.
- You're at higher risk if you have a history of acne, undergo high-density procedures, or don't follow aftercare instructions.
- Most cases are mild and heal completely without affecting your hair transplant results.
- Prevention focuses on following your surgeon's hygiene instructions and avoiding contamination.
- Treatment includes warm compresses, prescribed antibiotics, and maintaining proper scalp cleanliness.
- Contact your doctor if symptoms persist beyond 10 days, worsen, or you develop fever.
What Is Folliculitis After Hair Transplant?
Folliculitis after hair transplant is when the tiny pockets in your scalp where hair grows (called hair follicles) become inflamed or infected. This can happen in both the area where hair was removed (donor site) and where new hair was placed (recipient area) following your hair restoration surgery.
During your hair transplant procedure, whether FUE or FUT, your scalp's natural protective barrier gets disrupted. This creates small openings where bacteria can potentially enter the follicles, causing them to become red, swollen, and sometimes filled with pus.
Think of each hair follicle as a tiny tube in your skin. When these tubes become irritated or infected, your body's immune system responds by sending white blood cells to fight the problem, which causes the redness and swelling you see as folliculitis. While this might look concerning, most cases are superficial, affecting only the upper part of the follicle, and respond well to simple treatments.
What Does Folliculitis Look Like After Hair Transplant?
Recognizing folliculitis early helps you get appropriate treatment and prevents complications. The appearance progresses through several distinct stages that both patients and medical teams can easily identify.
- Early Warning Signs - Small, red bumps appearing around individual hair follicles with mild tenderness when you gently touch the affected areas.
- Progressive Development - White or yellow-headed bumps (pustules) forming at the center of red areas with increased redness spreading around each affected follicle.
- Advanced Symptoms - More noticeable tenderness that may interfere with sleep if you lie on the affected area, and possible mild swelling when several follicles are affected close together.
- Distribution Pattern - Folliculitis typically appears in scattered patches rather than covering your entire scalp, most commonly around newly transplanted grafts in the recipient area.
In your recipient area, you'll most likely see it around newly transplanted grafts, while in your donor area, it may develop around healing extraction sites or along your strip incision if you had FUT surgery.
How Common Is Folliculitis After Hair Transplant?
📊 Moderate Occurrence Rate
About 12.1% of hair transplant patients develop folliculitis during their recovery, making it one of the more common post-operative complications you might experience. However, your individual risk depends on several factors you can often control.
Most patients who develop folliculitis notice it within the first 1-3 weeks after surgery, with the highest likelihood occurring around days 7-14. This timing coincides with when scabs are forming and beginning to shed naturally. If you notice symptoms in the first week, it's often related to surgical trauma, while later cases usually stem from hygiene factors.
How Long Will Folliculitis Last After My Hair Transplant?
The duration of your folliculitis depends on how severe it is and how quickly you start treatment. Understanding the timeline helps set proper expectations for your recovery process.
Mild Cases
Usually starts 5-14 days after surgery and resolves completely within 7-10 days
Moderate Cases
May last 10-14 days total, improving within 5-7 days of using prescribed antibiotics
Severe Cases
Can persist for 2-3 weeks or longer, often requiring oral antibiotics
Recovery Factors
Timeline affected by treatment speed, immune response, and hygiene maintenance
What Causes Folliculitis After Hair Transplant?
Understanding what causes folliculitis helps you take steps to prevent it. Several factors can contribute to developing this condition during your hair transplant recovery.
Bacterial Overgrowth
The most common culprits are bacteria that normally live on your skin but can overgrow when your scalp's protective barrier is disrupted. Staphylococcus aureus is the most frequent cause, while patients with acne history may also deal with Propionibacterium acnes.
Surgical Factors
During your procedure, hair follicles can be damaged if grafts are handled roughly, placed too deep or shallow, or if there's excessive manipulation during placement. Poor bleeding control can also lead to clot formation around follicles, creating an environment for bacterial growth.
Post-Surgical Hygiene Issues
Waiting too long to wash, inadequate cleaning, overwashing with aggressive techniques, or using harsh or contaminated hair care products can all contribute to folliculitis development.
Environmental and Lifestyle Factors
Excessive sweating, touching your scalp, tight headwear that traps moisture, and pre-existing skin issues like seborrheic dermatitis or acne all increase your risk.
Am I at Higher Risk for Folliculitis After Hair Transplant?
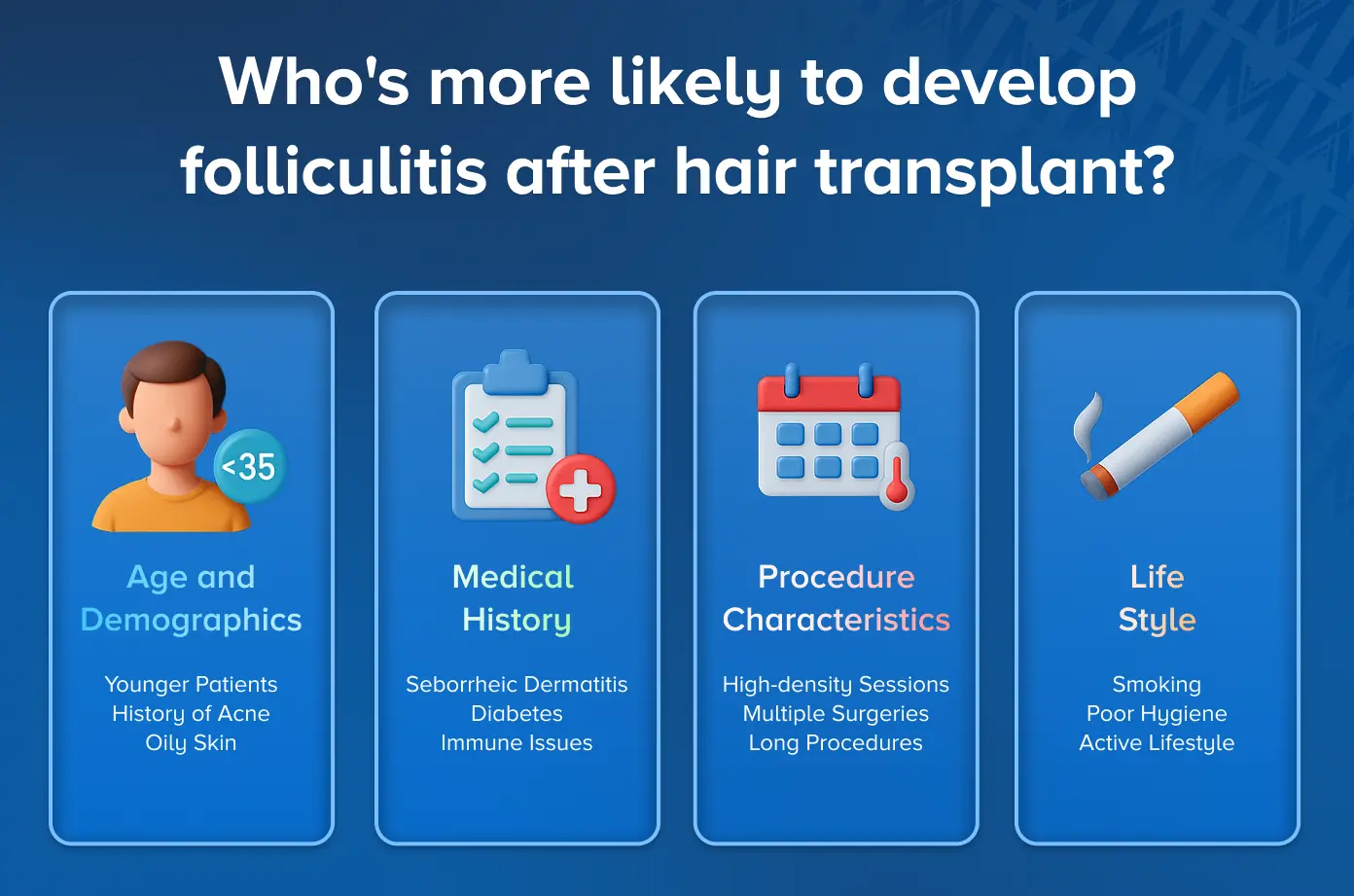
Certain factors make some patients more likely to develop folliculitis. Understanding your risk level helps you take extra precautions during your recovery period.
- Age and Demographics - Younger patients under 35 have higher risk, often due to increased oil production in the scalp and history of acne.
- Medical History - Seborrheic dermatitis, diabetes, immune system issues, or previous scalp surgery increase your risk.
- Procedure Characteristics - High-density sessions with more than 2,500 grafts, multiple procedures, long surgery times, or procedures in hot, humid environments.
- Lifestyle Factors - Poor hygiene habits, smoking, active lifestyle with quick return to sweating activities, or history of medication non-compliance.
How Will My Doctor Diagnose Folliculitis?
Your doctor will primarily diagnose folliculitis by examining your scalp and discussing your symptoms. The diagnostic process is typically straightforward and focuses on distinguishing folliculitis from other post-operative conditions.
Physical Examination
- Your doctor will look for characteristic red bumps or pustules centered around individual hair follicles
- They'll note the pattern of distribution, when symptoms started, and how the lesions appear compared to normal post-operative healing
- Assessment of timing and your response to any treatments already tried
Additional Testing When Needed
- If you have pustules, your doctor might take a small sample of the fluid to identify the specific bacteria causing your infection
- This helps them choose the most effective antibiotic for your situation
- Culture testing is particularly useful for severe or recurrent cases
How Serious Is Folliculitis After My Hair Transplant?
The seriousness of folliculitis varies, but understanding the different levels helps you know what to expect and when to seek additional medical attention.
⚠️ Severity Assessment
• Mild Cases (Most Patients): Only affects the surface of your follicles, won't impact your graft survival when treated promptly, heals completely without any scarring.
• Moderate Cases: Involves deeper inflammation but still manageable, may temporarily disrupt your normal hair growth cycle, could cause temporary hair loss that grows back.
• Severe Cases (Rare): Risk to your grafts through severe inflammation that can damage newly transplanted follicles, potential abscess formation requiring professional drainage.
The vast majority of patients who develop folliculitis and receive appropriate treatment see no lasting impact on their hair transplant success. The key is recognizing symptoms early and getting proper treatment promptly.
How Can I Prevent Folliculitis After Hair Transplant?
✅ Prevention Strategies
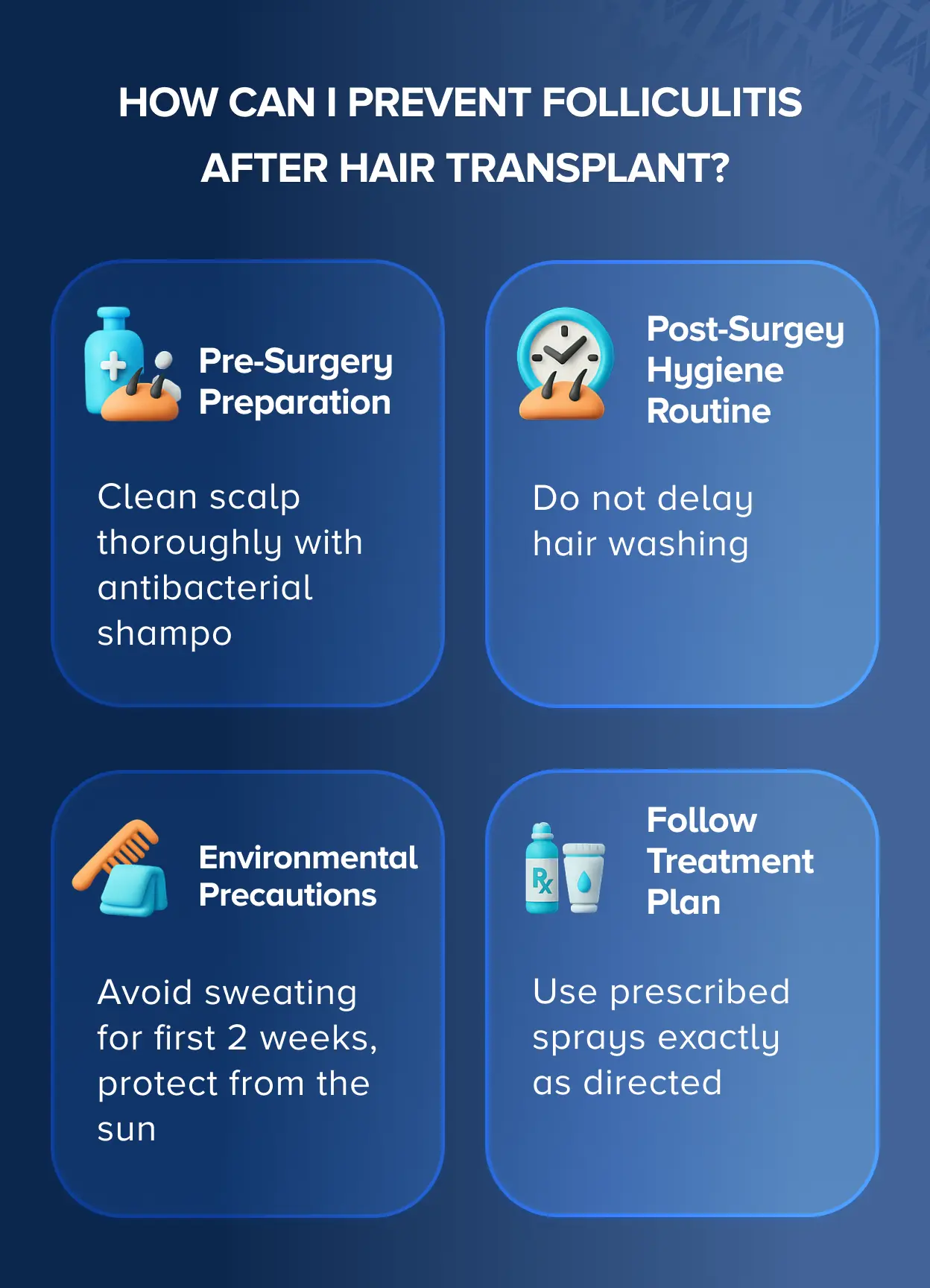
Preventing folliculitis requires following your surgeon's instructions carefully and maintaining excellent scalp hygiene:
- Pre-Surgery Preparation: Clean your scalp thoroughly with antibacterial shampoo, avoid hair products for 24-48 hours before surgery, and inform your surgeon about any history of acne or skin infections.
- Post-Surgery Hygiene Routine: Start washing when instructed (usually 24-48 hours after surgery), use only approved products, be extremely gentle with fingertips only, and rinse thoroughly.
- Daily Care Control: Keep your scalp clean with consistent, gentle daily washing, wash your hands before touching your scalp, use fresh pillowcases every night for the first week.
- Environmental Precautions: Avoid sweating for first 2 weeks, protect from sun but avoid tight-fitting hats, keep recovery area clean and well-ventilated, stay out of pools and hot tubs.
- Follow Treatment Plan: Use prescribed sprays exactly as directed, apply only surgeon-approved moisturizers, attend all scheduled follow-up appointments.
How Should I Treat Folliculitis After Hair Transplant?
Home Care Measures
- Warm compresses: Apply clean, warm, damp cloths to affected areas for 10-15 minutes, 3-4 times daily to reduce inflammation and help pustules drain naturally.
- Continue gentle washing: Keep using mild antibacterial shampoo as directed, being extra careful not to scrub.
- Don't pick or squeeze: Never try to pop pustules yourself, as this can worsen infection and cause scarring.
Medical Treatments
- Topical antibiotics: Medications like mupirocin or bacitracin that you apply directly to affected areas twice daily.
- Antiseptic solutions: Special cleansers like diluted chlorhexidine to help eliminate bacteria.
- Oral medications: For moderate to severe cases, oral antibiotics like cephalexin, clindamycin, or doxycycline.
Professional Interventions
- Drainage: Large pustules or abscesses may need professional drainage in your doctor's office.
- Culture testing: Testing pustule fluid to identify specific bacteria and choose the best antibiotic.
- Injection therapy: Severe inflammatory cases might benefit from anti-inflammatory injections.
Will My Folliculitis Go Away Completely?
Yes, folliculitis after hair transplant almost always resolves completely with proper treatment, and most cases don't affect your final hair transplant results. Folliculitis is typically a temporary complication that heals completely.
Recovery Timeline
- Mild cases: Usually resolve within 7-10 days with basic care
- Moderate cases: Clear within 10-14 days with prescribed antibiotics
- Severe cases: May take 2-3 weeks but still resolve completely with proper treatment
Impact on Hair Growth
- Folliculitis may temporarily slow or stop hair growth in affected follicles
- Once inflammation clears, normal hair growth typically returns to those areas
- Most cases don't cause lasting damage to your hair follicles
- Your final hair transplant results are typically unaffected by resolved folliculitis
When Should I Contact My Doctor About Folliculitis?
⚠️ When to Seek Medical Attention
While most folliculitis cases are manageable at home, certain warning signs require prompt medical attention:
• Call Immediately: Fever above 100.4°F (38°C), red streaking extending away from affected areas, severe pain that doesn't improve with over-the-counter pain relievers, large pustules larger than a pea, or feeling sick with chills and flu-like symptoms.
• Schedule Within 1-2 Days: No improvement after 5-7 days of treatment, spreading infection with new pustules in previously unaffected areas, multiple large, painful pustules developing simultaneously, or concerns about visible graft damage.
• Routine Follow-Up: Mild symptoms persisting beyond 10 days, treatment questions about proper medication use, recurring problems after initial clearing, or cosmetic worries about potential scarring.

