Hair Transplant Infection: Warning Signs, Prevention & Treatment
Of patients develop true infections after hair transplant surgery
Typical onset period after procedure
Response time to antibiotic treatment
Complete resolution with proper treatment
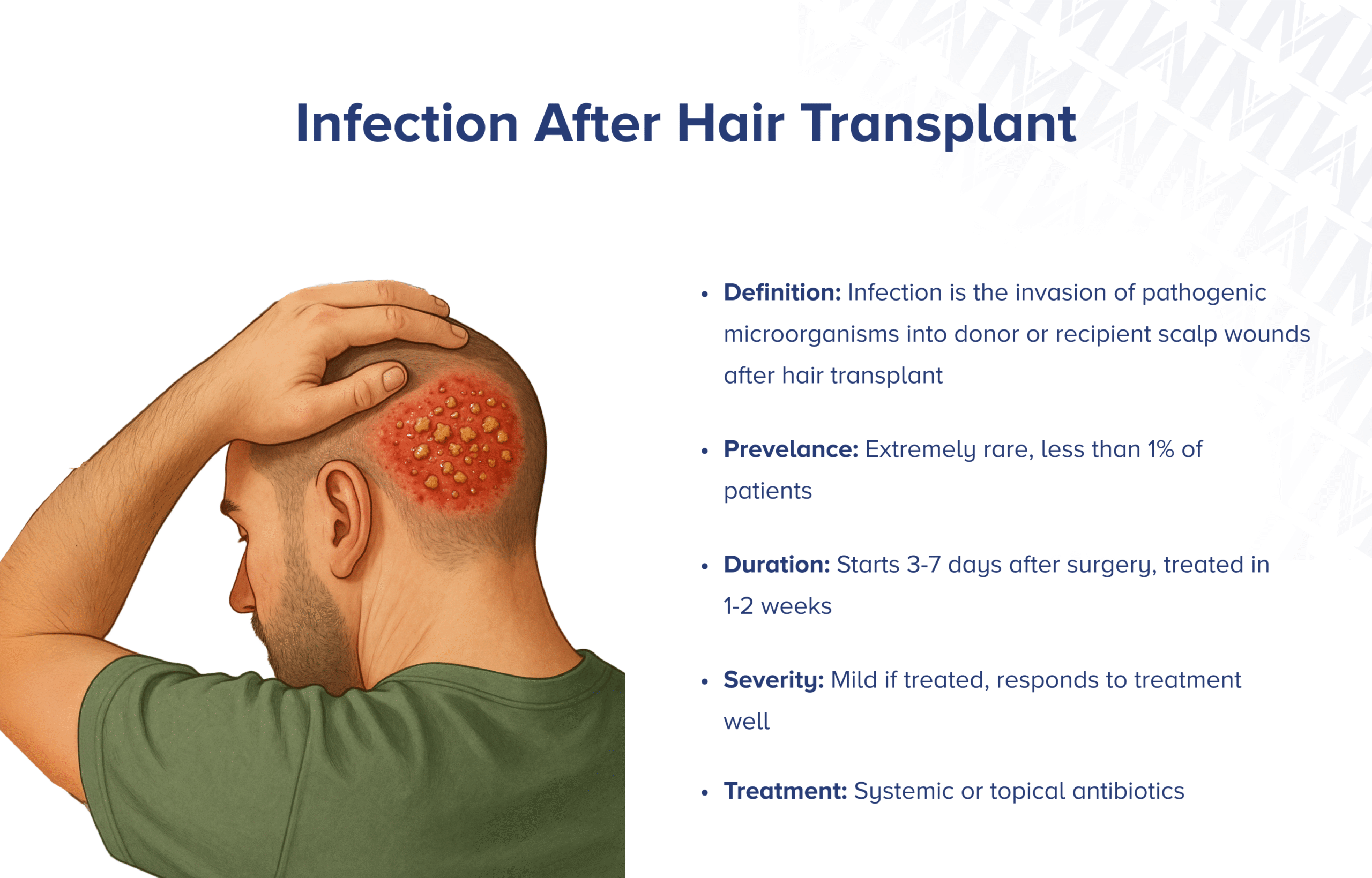
Hair transplant infection is a rare but serious complication where harmful bacteria invade the donor or recipient scalp wounds, causing inflammation, pus formation, and potentially threatening your graft survival. True postoperative hair transplant infections occur in less than 1% of hair transplant cases, typically developing 3-7 days after follicular unit extraction (FUE) or strip harvesting (FUT) procedures.
While infection after hair transplant is uncommon, understanding how to recognize early warning signs, prevent bacterial contamination, and seek prompt treatment is crucial for protecting your investment and ensuring optimal healing. Most infections respond well to antibiotic treatment when caught early, resolving completely within 1-2 weeks without affecting your final hair transplant results.
Key Points
- Infections after hair transplant are rare, occurring in less than 1% of patients undergoing hair restoration surgery.
- Symptoms typically appear 3-7 days after surgery and include increased redness, warmth, pain, and pus formation.
- Most infections resolve within 1-2 weeks with appropriate antibiotic treatment when caught early.
- Risk factors include diabetes, poor hygiene, excessive crusting, and immunosuppression.
- Prevention focuses on maintaining sterile conditions and following strict post-operative care instructions.
- Treatment involves antibiotics guided by bacterial culture results and possible drainage of abscesses.
- Prompt treatment prevents serious complications like graft loss, scarring, or systemic infection.
- Contact your doctor immediately if you notice increasing pain, fever, or pus formation.
What is a hair transplant infection?
Hair transplant infection is a bacterial contamination of the donor or recipient scalp sites following hair transplant surgery, characterized by pathogenic microorganisms invading healing wounds and causing inflammatory tissue damage beyond normal post-operative healing. Unlike normal healing inflammation, infection represents an active bacterial invasion that requires immediate medical treatment to prevent serious complications.
During your hair transplant procedure, your surgeon creates hundreds of tiny wounds in your scalp. While these are normally protected by your body's immune system and proper wound care, certain circumstances can allow bacteria to establish an infection. These harmful microorganisms multiply rapidly, producing toxins that damage surrounding tissue.
The difference between normal healing and infection is crucial to understand. Normal post-operative inflammation gradually improves each day, while infection causes worsening symptoms, including increased pain, spreading redness, warmth, and pus formation that doesn't resolve on its own.
What are the signs and symptoms of hair transplant infection?
Recognizing hair transplant infection early is critical for preventing further complications. Here's what to watch for:
Early warning signs of hair transplant infection:
- Increasing pain that gets worse instead of better after the first few days
- Spreading redness that extends beyond the donor and recipient areas
- Warmth when you touch affected areas, feeling noticeably hotter than the surrounding skin
- Swelling that increases rather than decreases over time
Progressive symptoms of hair transplant infection:
- Thick, yellow, or green pus discharge from graft sites or donor areas
- Foul-smelling drainage that has an unpleasant odor
- Red streaking extending away from infected areas
- Increased tenderness that makes it difficult to sleep or touch your scalp
Advanced hair transplant infection signs:
- Large, fluid-filled bumps (abscesses) that feel firm and painful
- Visible graft displacement or loss in infected areas
- Systemic symptoms like fever, chills, or feeling generally unwell
Normal healing involves gradually decreasing redness, pain, and swelling over the first week. In contrast, infection causes these symptoms to worsen after the initial 2-3 days.
How common is infection after hair transplant?
📊 Extremely Rare Occurrence
Infection after hair transplant is rare, occurring in less than 1% of patients undergoing hair transplant surgery. This low incidence reflects the effectiveness of modern sterile surgical techniques and improved post-operative care protocols.
Why hair transplant infections are so rare:
- Modern hair transplant clinics maintain operating room-level sterility
- Experienced surgeons use minimally invasive methods that reduce tissue trauma
- Many surgeons prescribe preventive antibiotics for high-risk patients
- Improved post-operative care instructions help patients avoid contamination
Most infections that do occur develop within the first week after surgery, with peak incidence between days 3-7. After the first 10 days, your risk of complications drops dramatically as your wounds begin to heal and seal. By three months post-surgery, the risk becomes negligible as healing is complete.
How long does an infection last after a hair transplant?
The duration of hair transplant infections depends on how quickly you recognize symptoms and begin appropriate treatment. Early intervention dramatically affects both healing time and final outcomes.
Typical Timeline:
Onset: Most infections become apparent 3-7 days after surgery
Treatment response: With appropriate antibiotics, improvement usually begins within 24-48 hours
Resolution: Most infections resolve completely within 1-2 weeks of starting treatment
Mild Infections: Usually resolve within 5-7 days with oral antibiotics
Moderate Infections: May require 10-14 days of treatment for complete resolution
Severe Infections (Rare): Can take 2-3 weeks or longer to fully resolve
Early antibiotic therapy dramatically shortens infection duration. Once your infection clears, your scalp typically heals normally, though severe infections may leave some scarring.
What causes infection after hair transplant?
Several factors can contribute to developing a hair transplant infection, ranging from post-operative care issues to individual patient risk factors.
Post-Operative Hygiene Issues
Delayed washing allows bacteria to multiply, using contaminated water or dirty towels, touching the scalp with dirty hands transfers bacteria to healing wounds, and keeping wounds moist for extended periods promotes bacterial growth.
Wound Care Problems
Excessive crusting can harbor bacteria and delay healing, tight closures can reduce blood flow and impair healing, and poor bleeding control during surgery can create blood clots that bacteria can colonize.
Patient Risk Factors
A compromised immune system from diabetes, autoimmune diseases, or medications, poor circulation from smoking or vascular disease, nutritional deficiencies needed for wound healing, and chronic skin conditions like severe seborrheic dermatitis.
Environmental Contamination
Using dirty pillowcases or hats against your healing scalp, swimming or using a hot tub before wounds are sealed, and contact with pets that may carry harmful bacteria.
Who is more likely to develop an infection after a hair transplant?
Certain factors increase your likelihood of developing an infection after a hair transplant. Understanding these risk factors helps both patients and medical teams implement appropriate preventive measures.
- Medical Conditions - Diabetes with high blood sugar levels that impair wound healing, autoimmune diseases like lupus that compromise infection-fighting ability, cancer or chemotherapy treatments that suppress the immune system.
- Medications - Immunosuppressive drugs like steroids or organ transplant medications, blood thinners that increase bleeding and complicate wound healing, chronic antibiotics that can lead to resistant bacterial infections.
- Lifestyle Factors - Smoking that dramatically reduces blood flow to healing tissues, excessive alcohol use that interferes with wound healing and immune function, poor nutrition with inadequate protein, vitamin C, or zinc.
- Procedural Risk Factors - Large sessions involving many grafts creating more wounds for potential infection, multiple procedures in previously treated areas, complications during surgery like excessive bleeding or prolonged procedure time.
How is a hair transplant infection diagnosed?
Your doctor will diagnose hair transplant infection through careful examination and possibly laboratory testing to distinguish true infection from normal healing processes or other complications.
Physical Examination
Your doctor will inspect your scalp for spreading redness, swelling, warmth, and purulent discharge. They'll gently feel the affected areas to check for fluid-filled areas, increased warmth, and tenderness.
Key Diagnostic Signs
- Progressive worsening symptoms that get worse rather than better over time
- Purulent discharge with thick, yellow or green drainage
- Surrounding cellulitis with red streaking beyond immediate surgical sites
- Systemic symptoms like fever or feeling unwell
Laboratory Testing (When Needed)
If your doctor suspects infection, they may collect a sample of any discharge for bacterial culture and sensitivity testing. This identifies the specific bacteria and determines which antibiotics will be most effective.
Your doctor will differentiate true infection from normal post-operative inflammation, allergic reactions, or folliculitis based on the pattern of symptoms and extent of surrounding inflammation.
How serious is a hair transplant infection?
The seriousness of a hair transplant infection varies from mild cases that respond quickly to antibiotics to severe infections that can threaten your health and surgical results.
⚠️ Infection Severity Assessment
• Mild Infections (Most Common): Limited to small areas of your scalp, respond quickly to oral antibiotics, don't typically affect graft survival when treated promptly, heal completely without lasting effects.
• Severe Infections (Rare but Serious): Graft loss where severe infection can kill newly transplanted follicles, abscess formation requiring surgical drainage, extensive scarring that creates permanent damage.
• Systemic Complications: Bacteria can enter your bloodstream requiring hospitalization, potential for cellulitis spreading to surrounding tissues, rare but serious complications affecting overall health.
Most infections cause only brief disruption to healing when treated promptly. The vast majority of patients who receive prompt treatment maintain excellent results and complete healing without long-term complications.
How to prevent hair transplant infections?
✅ Prevention Strategies
Preventing hair transplant infections requires diligent attention to hygiene and following your surgeon's instructions:
- Pre-Operative Preparation: Use prescribed chlorhexidine or antibacterial shampoo before surgery, avoid hair products, salons, or swimming for 48 hours before surgery, control diabetes, stop smoking, and ensure adequate nutrition.
- Daily Hygiene Protocol: Use only surgeon-approved shampoos and lukewarm water, wash with fingertips using light pressure, ensure complete removal of all soap, blood, and debris, pat dry with fresh, clean towels.
- Environmental Precautions: Use fresh pillowcases daily and wash bedding in hot water, stay out of pools, hot tubs, lakes, or oceans for at least 2 weeks, avoid close contact with animals that might carry harmful bacteria.
- Nutritional Support: Ensure sufficient protein intake for wound healing, include vitamin C through citrus fruits and vegetables, stay hydrated and limit alcohol consumption during initial healing.
How to treat a hair transplant infection?
Immediate Steps
- Contact your surgeon immediately: Don't wait to see if symptoms improve - early intervention is crucial for optimal outcomes.
- Document symptoms: Take clear photos and notes about progression to help your medical team assess severity.
- Avoid self-treatment: Don't use over-the-counter antibiotics without professional guidance.
- Continue gentle hygiene: Maintain proper scalp care while awaiting medical evaluation.
Antibiotic Treatment
Your doctor will prescribe antibiotics based on the suspected bacteria and severity. Common choices include oral antibiotics like cephalexin, clindamycin, or doxycycline for mild to moderate infections, or IV antibiotics for severe cases.
Taking Antibiotics Properly
- Finish all prescribed medication: Complete the full course even if symptoms improve
- Maintain consistent timing: Take doses at evenly spaced intervals
- Don't skip doses: This prevents bacterial resistance development
- Report side effects: Contact your doctor about any adverse reactions
Local Wound Care
- Apply clean, warm, damp cloths: Use for 10-15 minutes several times daily
- Continue prescribed cleansers: Be extra gentle around infected areas
- Allow natural drainage: Don't squeeze or manipulate wounds
- Use light dressings: Apply breathable coverings if recommended
Expected Timeline
You should notice initial improvement within 24-48 hours of starting antibiotics, with significant reduction in symptoms by 3-5 days and substantial resolution within 7-10 days.
Will a hair transplant infection go away completely?
Yes, the vast majority of infections after hair transplant resolve completely with prompt, appropriate treatment, and most patients maintain excellent hair transplant results. Recovery follows a predictable timeline with proper medical intervention.
Recovery Timeline
- Initial improvement: Reduced pain and redness within 24-48 hours of starting antibiotics
- Progressive healing: Symptoms continue improving over the first week
- Complete resolution: Most infections heal completely within 10-14 days
- Return to normal: Your scalp typically returns to normal healing patterns once infection clears
Impact on Hair Transplant Results
- Most infections don't affect final outcomes when treated promptly
- Hair growth might be slightly delayed in previously infected areas
- Hair follicles typically resume normal growth once infection resolves
- The majority of patients achieve their expected results
When to see a doctor for hair transplant infections?
⚠️ When to Seek Medical Attention
Recognizing when to seek medical attention for hair transplant infections can prevent serious complications:
Contact Your Doctor Immediately If You Experience:
- Increasing pain: Pain that gets worse instead of better after the first 2-3 days
- Spreading redness: Red areas that extend beyond surgical sites or develop red streaking
- Purulent discharge: Thick, yellow, or green drainage with or without odor
- Fever: Temperature above 100.4°F (38°C) or feeling generally unwell
- Rapid worsening: Any symptoms that worsen quickly over a few hours
Emergency Situations (Seek Immediate Care):
- High fever above 100.4°F (38°C) accompanied by chills or severe illness
- Severe headache with neck stiffness or sensitivity to light
- Rapidly spreading infection across large areas of your scalp
- Signs of sepsis including confusion, rapid heart rate, or difficulty breathing
Schedule an Appointment Within 24 Hours If:
- Persistent symptoms that don't improve after 5-7 days
- New pustules in previously unaffected areas
- Symptoms that initially improved but then worsen again
- Visible loss or displacement of transplanted hair in infected areas
Information to Provide Your Doctor:
- Exactly when you first noticed each symptom and how they've progressed
- All treatments you've been using, including over-the-counter products
- Photos showing the progression of your condition
- Any fever, chills, or feeling unwell
Your surgical team wants to address any issues promptly. It's always better to contact them early with concerns rather than wait and risk complications. Early intervention almost always leads to better outcomes and protects your hair transplant investment.