Post-hair-transplant erythema (redness) is a short-lived inflammatory response driven by microvascular dilation and leukocyte influx at donor and recipient incisions after FUT or FUE hair transplant procedures. Redness after a hair transplant can be classified into three types: mild (physiological vasodilatory flushing), moderate (sterile perifollicular inflammation), and severe (infectious cellulitis or folliculitis).
A multicenter review of 1,090 hair-transplant patients from the Aesthetic Plastic Surgery journal showed that 22.4% (about 1 in 5) of hair transplant patients developed recipient-area perifollicular erythema; 16% mild, 5% moderate, and less than 1% severe. Post-hair transplant redness was tied to significantly greater hair-shaft shedding and lower graft survival. Folliculitis raised the odds of mild and moderate post-hair transplant redness about six and three times, respectively, while postponing the first postoperative hair wash increased the risk of moderate and severe post-hair transplant redness.
Most cases of redness after a hair transplant typically resolve within a timeframe of 2 to 4 weeks. However, various factors can affect both the severity and duration of inflammatory responses. Implementing effective prevention strategies and initiating early treatment interventions are crucial, as they can significantly alleviate discomfort and promote the best possible graft survival and aesthetic outcomes.
Key Points
- Affects 22.4% of hair transplant patients with varying severity levels - 16% mild, 5% moderate, and less than 1% severe cases.
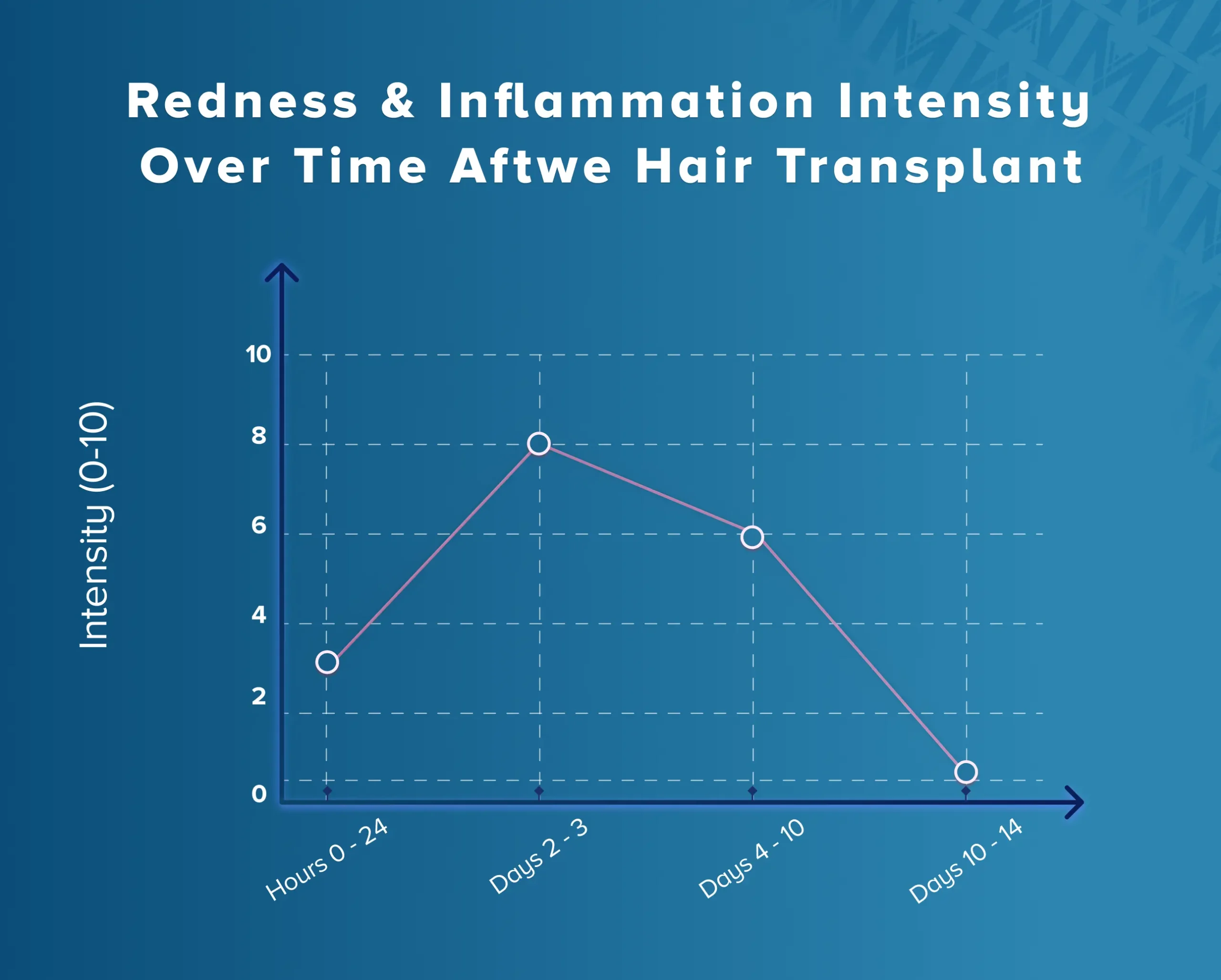
- Redness peaks 2-3 days post-surgery and typically resolves within 10-14 days for most patients.
- Fair-skinned patients and large graft sessions increase the risk of developing noticeable erythema.
- Folliculitis significantly increases risk - raising odds of mild inflammation by six times and moderate inflammation by three times.
- Delayed first washing beyond recommended timeframes increases risk of moderate and severe inflammatory responses.
- Prevention strategies include gentle tissue handling, proper surgical technique, and appropriate postoperative care timing.
- Treatment options range from cool compresses and topical treatments to oral corticosteroids for severe cases.
- Medical evaluation is needed if symptoms worsen, spread beyond transplant sites, or persist beyond 2 weeks.
- Redness is generally self-limited and resolves without lasting effects on graft survival or aesthetic outcomes.
- Seek immediate attention for signs of infection like purulent discharge, fever, spreading redness, or severe pain.
What is redness and inflammation after hair transplant?
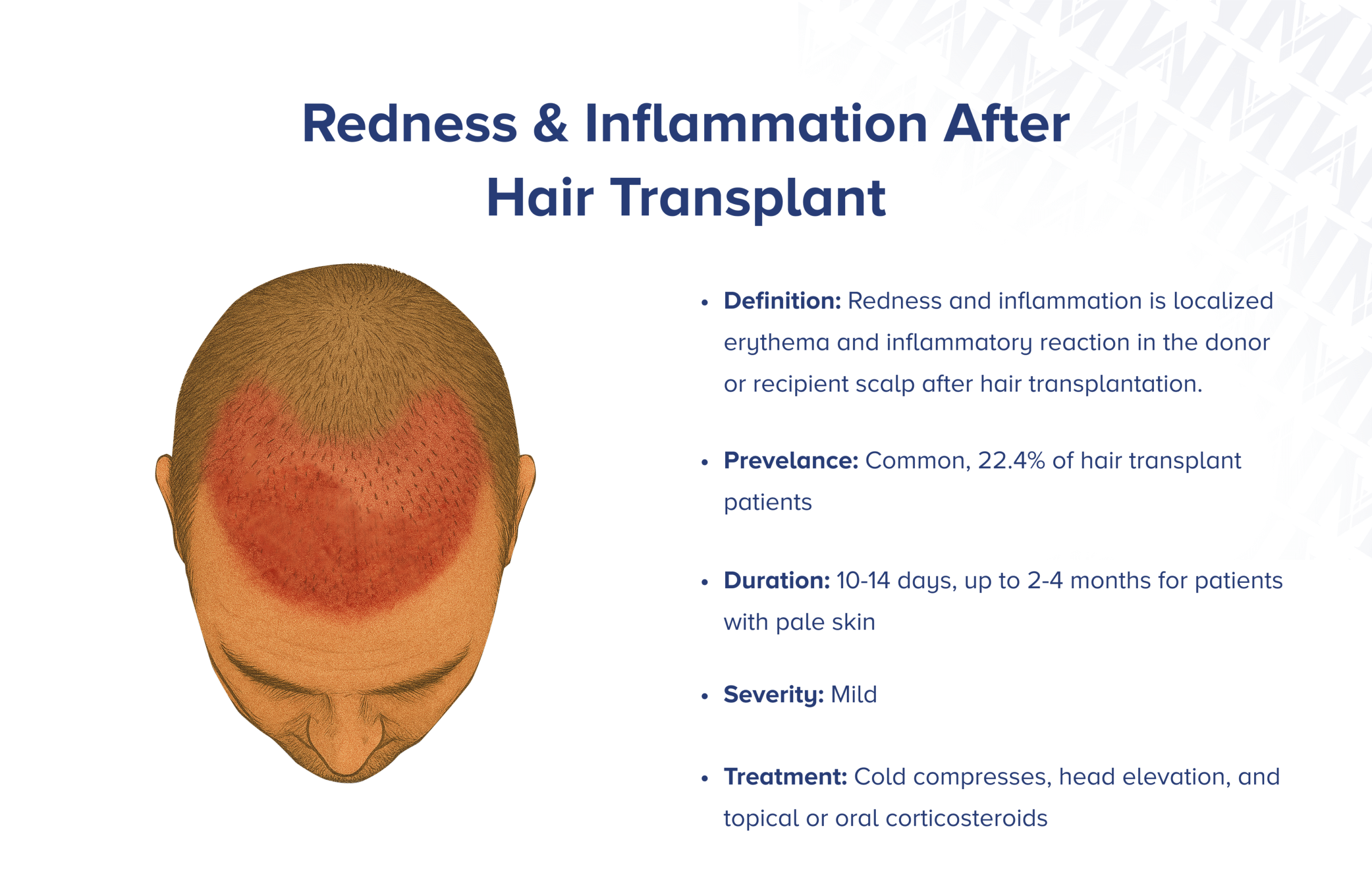
Redness after hair transplant involves localized erythema and inflammatory reactions that occur in the donor or recipient scalp following surgical intervention. These responses result from surgical trauma-induced capillary dilation and immune cell infiltration, which are part of the body's natural healing process.
Mechanisms of Redness Formation
1. Inflammatory Cascade Response
The inflammatory cascade starts right after graft extraction and implantation, as tissue damage releases mediators like histamine, prostaglandins, and cytokines. This causes blood vessels to dilate and become more permeable, resulting in redness, warmth, and mild swelling around transplanted areas.
2. Physiological Healing Process
This physiological response aids wound healing by boosting blood flow to damaged tissues, delivering essential nutrients, oxygen, and immune cells. Though concerning for patients, these reactions usually indicate normal healing rather than complications.
3. Microvascular Changes
Surgical trauma creates micro-wounds during follicular unit extraction and recipient site preparation, initiating reactions that recruit inflammatory cells for healing. These changes in small blood vessels lead to the characteristic redness and warmth observed in the treated areas.
What are the signs of redness and inflammation?
The signs include visible erythema (redness) of the scalp accompanied by warmth, tenderness, and sometimes mild swelling around individual graft sites. These symptoms typically appear within hours of surgery and may intensify over the first few days before gradually subsiding.
- Visible redness (erythema) - Pinkish to red discoloration extending beyond immediate transplant sites, particularly noticeable in fair-skinned individuals where vascular changes become more apparent.
- Warmth - Affected areas feel noticeably warm to the touch due to increased blood flow to healing tissues.
- Tenderness - Mild to moderate discomfort when gentle pressure is applied to transplanted areas.
- Localized swelling - Subtle tissue elevation around individual grafts rather than widespread edema, reflecting the targeted nature of follicular unit transplantation.
- Papules or pustules - Small elevated lesions that may develop if secondary folliculitis occurs, representing inflammatory reactions around individual hair follicles.
- Sensory changes - Mild itching or tingling sensations as nerve endings regenerate and tissues heal, typically indicating normal healing progression.
Mild Redness (16.33%)
Light pink to red coloration confined to hair transplant sites with minimal warmth, slight tenderness only with direct pressure, and no visible swelling. Resolves within 7-10 days without intervention.
Moderate Redness (5.14%)
More pronounced redness extending beyond graft sites with noticeable warmth, moderate tenderness, mild swelling, and possible small papules. May persist 2-3 weeks and benefit from topical treatment.
Severe Redness (0.92%)
Intense erythema with possible spreading, significant warmth and swelling, marked tenderness, pustules or infection signs, and possible systemic symptoms like fever. Requires medical evaluation.
How common is redness after hair transplant?
📊 Prevalence Statistics
Redness and inflammation occur in approximately 22.4% (about 1 in 5) of hair transplant patients, with the majority experiencing mild forms of these reactions. According to clinical studies, 16.33% of patients develop mild perifollicular erythema, 5.14% experience moderate redness, and 0.92% present with severe redness and inflammatory responses.
Recipient area inflammation is more common than donor site reactions due to the dense graft placement and significant tissue manipulation during implantation. This localized surgical trauma triggers inflammatory responses, with susceptibility varying based on genetic factors, skin type, and healing characteristics.
How long does redness and inflammation last?
Redness and inflammation usually peak 2-3 days after hair transplant surgery and fade within 10-14 days for most patients. However, fair-skinned individuals or those with large grafts may experience erythema lasting 2-4 months.
Initial Phase (Hours-24h)
Inflammatory response begins within hours of surgery as tissue trauma releases inflammatory mediators. Mild redness and warmth appear around graft sites as part of the natural healing cascade.
Peak Phase (Days 2-3)
Maximum inflammatory activity occurs with peak redness, warmth, and possible swelling. This marks the height of the healing response as blood flow increases and immune cells arrive at transplant sites.
Decline Phase (Days 4-10)
As the healing progresses, inflammatory mediators decrease and blood vessel permeability normalizes. Improvements are usually seen by the end of the first week with gradual fading of redness.
Resolution (Days 10-14)
Complete resolution of inflammatory signs for most patients. Any remaining mild erythema typically fades completely, with tissues returning to normal appearance and comfort levels.
What causes redness and inflammation after hair transplant?
Understanding the causes of redness helps in both prevention and effective management of post-transplant inflammatory responses:
- Mechanical trauma from graft extraction and implantation triggers the release of pro-inflammatory mediators in affected tissues, initiating the healing cascade that produces redness and warmth.
- Surgical process creates micro-wounds during follicular unit extraction and recipient site preparation, initiating reactions that recruit inflammatory cells for healing and tissue repair.
- Anesthetic injections further contribute to tissue trauma, adding to the inflammatory burden and contributing to the overall erythematous response in treated areas.
- Individual immune responses significantly influence inflammation intensity; patients with hyperactive immune systems or those on specific medications may react more strongly to surgical trauma.
- Secondary bacterial colonization can worsen inflammation if postoperative hygiene is not maintained, leading to folliculitis and increased erythema around graft sites.
- Environmental factors like sun exposure and chemical irritants can heighten inflammation during the early healing period, prolonging redness and discomfort.
Who is more likely to get redness after hair transplant?
Patients at higher risk for redness and inflammation include those with lighter skin types, individuals undergoing large-session procedures, patients who wash too early or too late post-operatively, and those with a history of folliculitis or sensitive skin conditions.
- Fair-skinned individuals (Fitzpatrick skin types I and II) tend to exhibit more noticeable inflammatory responses due to lower melanin levels, making erythema more pronounced compared to darker skin types.
- Larger graft sessions with over 3,000 follicular units can lead to significant tissue trauma and increased inflammation. More incisions and longer surgeries heighten tissue stress and the healing process.
- Delaying washing beyond 1-3 days increases the risk of moderate to severe post-operative erythema due to thick crusts and dried exudate on the scalp, which can cause irritation and lead to folliculitis.
- People with skin conditions like seborrheic dermatitis, psoriasis, or folliculitis may have heightened inflammation due to a weakened skin barrier and altered immune responses.
- Advanced age can affect inflammation, as older patients may experience longer healing times due to reduced cellular regeneration and slower immune responses.
- Previous history of folliculitis significantly elevates risk, raising the odds of mild inflammation by approximately six times and moderate inflammation by three times compared to patients without follicular complications.
How do doctors diagnose redness after hair transplant?
Diagnosis of redness and inflammation is primarily clinical, relying on visual inspection and physical examination:
1. Clinical Assessment
Healthcare providers evaluate the extent and progression of inflammation through physical examination, focusing on skin color changes, temperature elevation, and patient-reported discomfort confined to affected areas. The examination shows erythema, warmth, and tenderness without systemic infection signs.
2. Differential Diagnosis
When infection is suspected due to increased pain, purulent discharge, or spreading erythema, bacterial cultures or tissue biopsies may be done to identify pathogens and guide antibiotic choice. Differential diagnoses may include contact dermatitis, allergic reactions, or underlying skin conditions.
3. Severity Grading
Clinicians grade the severity as mild, moderate, or severe based on the extent of erythema, presence of swelling, patient discomfort levels, and any signs of secondary complications like folliculitis or infection.
4. Monitoring Progress
Regular follow-up assessments track the progression of healing and identify any worsening symptoms that might indicate complications requiring additional intervention or treatment modifications.
How serious is redness after a hair transplant?
Most cases of redness and inflammation are mild and resolve without treatment, though severity varies, influencing treatment approaches and potential complications. The seriousness depends on the grade and associated symptoms.
⚕️ Severity Assessment
Mild redness (16.33% of patients): Light pink to red discoloration with slight warmth and tenderness, minimal swelling, resolving within 7-10 days without intervention, indicating normal healing with little impact on aesthetics or graft survival.
Moderate redness (5.14% of patients): Pronounced redness beyond graft sites with noticeable warmth, moderate tenderness, mild to moderate swelling, and possible small papules lasting 2-3 weeks. Closer monitoring and possible topical treatment are advised.
Severe redness (0.92% of patients): Intense erythema with warmth, swelling, tenderness, and signs of infection like pustules. Systemic symptoms such as low-grade fever may arise, requiring immediate medical evaluation and potential antibiotic therapy.
How to prevent redness after a hair transplant?
Prevention of redness and inflammation involves using gentle tissue handling techniques, proper timing of postoperative care, and implementing evidence-based protocols to minimize inflammatory responses.
✅ Prevention Strategies
1. Gentle surgical technique using sharp punches for extraction, following proper graft handling protocols, and limiting manipulation of follicular units to minimize tissue trauma and inflammation.
2. Anti-inflammatory anesthetic preparation by adding corticosteroids such as triamcinolone to tumescent anesthetic solutions to blunt inflammatory responses during and after surgery.
3. Optimal washing timing by delaying the first postoperative wash until 48-72 hours after surgery to allow initial healing while preventing excessive crust buildup.
4. Minimizing surgical trauma through precise incision techniques, appropriate graft placement depth, and avoiding excessive tissue manipulation during the procedure.
5. Patient education on postoperative care including proper washing techniques, activity restrictions, and recognition of signs needing medical attention to prevent complications.
6. Pre-operative assessment to identify high-risk patients with skin sensitivities or previous folliculitis history, allowing for tailored preventive measures.
How to reduce redness after a hair transplant?
If redness occurs despite preventive measures, follow these evidence-based steps to manage inflammatory responses:
- Apply cool compresses - Use ice packs wrapped in thin towels for 10-15 minute intervals several times daily to reduce blood flow and provide immediate symptom relief.
- Sleep with head elevated - Maintain 30-45 degrees elevation above heart level for the first few nights to promote lymphatic drainage and reduce swelling.
- Follow gentle washing protocols - Begin gentle cleansing within 1-3 days using mild, hypoallergenic shampoo to prevent crust buildup and reduce irritation.
- Avoid sun exposure - Protect treated areas from direct sunlight and heat sources that can worsen inflammation and prolong redness.
- Stay hydrated - Drink plenty of water to support natural healing processes and reduce inflammatory responses throughout the body.
- Avoid touching or scratching - Resist the urge to touch treated areas to prevent bacterial introduction and additional trauma that can worsen inflammation.
For moderate to severe cases, topical corticosteroids such as hydrocortisone cream effectively reduce inflammation, while oral anti-inflammatory medications like prednisone are used for more severe responses. If folliculitis develops, topical antibiotics like mupirocin and oral antibiotics like cephalexin help control bacteria and reduce inflammation.
Will redness go away after a hair transplant?
The prognosis for post-transplant redness is overwhelmingly positive, with complete resolution expected in the vast majority of cases:
- Complete Resolution Within 2-4 Weeks: Most patients experience complete resolution of erythema as inflammatory mediators decrease and tissues heal. Normal skin color and appearance return without lasting effects on aesthetics.
- No Long-Term Impact on Graft Survival: Normal postoperative redness does not affect the survival or growth of transplanted hair follicles. While inflammation may temporarily mask grafts, it has no negative impact on long-term hair growth outcomes.
- Minimal Lasting Effects: After redness resolves, tissues return to their normal appearance and function. Any temporary skin sensitivity or slight color variations typically normalize completely.
- Psychological Relief: As inflammatory signs fade, patients often experience improved confidence and satisfaction with their procedure, enhancing overall treatment satisfaction and recovery experience.
When should you see a doctor for redness after hair transplant?
⚠️ Warning Signs Requiring Medical Attention
Most redness after hair transplant surgery is normal, but certain signs require prompt medical evaluation:
• Worsening or spreading redness beyond transplant sites, especially with red streaks, may indicate cellulitis or systemic infection requiring immediate antibiotic treatment.
• Redness persisting beyond 2 weeks without improvement may signal treatment-resistant infection, allergic reactions, or underlying skin conditions requiring specialized care.
• Severe pain or increasing discomfort especially with throbbing or pulsating sensations, may suggest complications like infection or tissue necrosis.
• Purulent discharge or unusual odors from transplant sites can signal bacterial infection requiring culture-guided antibiotic therapy and possible drainage.
• Systemic symptoms like fever, chills, or malaise accompanying redness may indicate serious infection requiring immediate medical assessment and treatment.
• Development of pustules or abscesses around graft sites requires evaluation for folliculitis or deeper tissue infection that may threaten graft survival.

