Hair transplant side effects, complications, and risks refer to the physiological and procedural consequences that may arise from surgical hair restoration methods such as Follicular Unit Extraction (FUE), Direct Hair Implantation (DHI), and Follicular Unit Transplantation (FUT). Side effects are typically expected and self-limiting biological responses, while complications denote medically significant conditions requiring intervention.
Most hair transplant patients experience normal side effects like swelling (42.5% of patients), shock loss (45% of patients), and mild discomfort as part of the natural healing process. These expected reactions typically resolve within 1-2 weeks without medical intervention.
Complications such as folliculitis, graft necrosis, or postoperative infection occur in less than 5% of patients, with documented infections reported in under 1%. These complications are typically associated with suboptimal technique, patient comorbidities, or non-compliance with aftercare.
Here are the key points:
- Side effects affect most patients as expected, temporary reactions lasting 1-2 weeks
- Complications requiring medical treatment occur in less than 5% of patients
- Infection rates are extremely low at less than 1% of cases
- Shock loss temporarily affects 45% of patients with complete regrowth expected
- Swelling occurs in 42.5% of patients, typically resolving within 1-2 weeks
- Pain significantly affects only 3.3% of patients after surgery
- Graft survival rates exceed 90% in modern hair transplant procedures
- Age, hair type, and skin characteristics significantly influence complication risks
- Proper aftercare prevents most complications and ensures optimal healing
Defining what a side effect, complication, or risk is for hair transplant
The difference between side effects, complications, and risks lies in their expected nature, severity, and treatment requirements. Side effects are expected and temporary, complications are unexpected medical problems requiring intervention, and risks are broader treatment considerations affecting overall outcomes.
Side effects are expected, mild events that resolve mostly without treatment, including swelling, scabbing, temporary shedding, and mild pain occurring within days and disappearing within 1-2 weeks. Side effects affect most patients as part of normal healing.
Complications are unintended adverse outcomes requiring medical intervention, including infections, significant scarring, skin necrosis, and graft failure. Complications affect less than 5% of patients and may require antibiotics or surgical revision.
Risks are non-medical considerations affecting satisfaction, budget, or lifestyle, including multiple sessions needed, unnatural appearance, and ongoing maintenance requirements. Risks represent potential outcomes that patients should consider, but do not constitute medical adverse events.
Common Causes for Hair Transplant Side Effects and Complications
- Surgeon Inexperience & Wrong Clinic Choice: Technical errors, overharvesting, poor incision depth or angle, inadequate asepsis, are far more common with less-experienced surgeons or substandard clinics, driving higher rates of graft damage, cobblestoning, and unnatural results.
- Poor Post-Op Hygiene & Aftercare Adherence: Neglecting scalp cleansing, head-elevation, medication schedules, or activity restrictions markedly increases risks of folliculitis, infection, graft loss, and scarring.
- Pre-Existing Scalp Conditions: Active acne, seborrheic dermatitis, or other inflammatory disorders predispose to folliculitis and delayed healing around grafts.
- Smoking: Nicotine-induced vasoconstriction compromises scalp blood flow, raising the odds of skin necrosis, poor graft take, and hypertrophic scarring.
- Diabetes & Hypertension: Microvascular disease and impaired immunity slow wound healing, heighten infection risk, and predispose to necrosis or dehiscence.
- Anticoagulant Use (Blood Thinners): Medications like warfarin or aspirin lead to prolonged bleeding and hematoma formation if not managed perioperatively.
What are the side effects of hair transplant?
- Shock Loss
- Swelling
- Pain & Discomfort
- Redness & Inflammation
- Tenderness
- Mild Bruising
- Minor Bleeding
- Scabbing
- Itching
- Temporary Numbness
- Syncope
- Hiccups
Shock Loss

Shock loss (recipient site effluvium) is a temporary shedding of hair that occurs in 45% of hair transplant patients, causing sudden hair shedding and visible thinning in the transplant area, noticed during washing or combing.
This common side effect typically occurs 2-6 weeks after surgery, when surgical stress interrupts the hair growth cycle. Most hair grows back completely within 3-4 months, with no lasting effects. Shock loss can be identified by diffuse hair shedding in the transplant area 2-6 weeks post-surgery, diagnosed by a positive hair-pull test and examination.
The temporary condition can be prevented and treated by starting topical minoxidil or oral finasteride within two weeks of surgery. Shock loss is more common in female patients and those with already thinning hair before surgery. You should see a doctor if hair shedding continues beyond six months, worsens unexpectedly, or occurs with scalp pain, redness, or signs of infection.
Learn More About Shock LossSwelling
Swelling (edema) after hair transplant surgery is an excess fluid buildup, causing visible puffiness and tightness in the scalp and eye area, affecting 42.5% of patients.
This temporary side effect begins within 24-48 hours, peaks around day 3, and resolves within 1-2 weeks. Swelling occurs when surgery damages blood vessels, making them leak and preventing lymphatic fluid from draining properly. This causes fluid to build up in the surrounding tissues.
Risk factors include larger procedures, older age, and heart or kidney conditions. Diagnosis involves visual inspection and physical examination to confirm fluid accumulation and temporary denting when pressed.
Swelling ranges from mild localized puffiness to severe cases that may impact vision and require medical intervention. Prevention and treatment include keeping the head elevated above heart level, applying cold compresses, and using anti-inflammatory medications, with corticosteroids reserved for severe cases.
Seek medical attention if swelling is sudden, severe, persists beyond 10 days, or occurs with pain, redness, warmth, or fever, as these symptoms may indicate complications requiring immediate intervention.
Learn More About SwellingPain & Discomfort

Pain and discomfort after hair transplant surgery are unpleasant sensations like tenderness, aching, or throbbing at donor and recipient sites, affecting only 3.3% of patients to a significant degree.
Pain after hair transplant peaks within 24 hours and resolves by day 3 for FUT patients and day 1 for FUE patients, with most feeling better within a week and less than 1% experiencing chronic pain.
Pain after hair transplant results from tissue trauma during graft harvesting, local anesthetic injections, wound tension from strip removal, and bleeding. Risk factors include FUT hair transplant, large surgical sessions, inadequate anesthesia, and significant wound tension.
Diagnosed using patient-reported pain scales, pain is typically mild to moderate (1-3/10 scores) and resolves without treatment, though rare chronic nerve pain requires specialized care. Treatment includes acetaminophen and NSAIDs as first-line therapy, with cold compresses providing additional relief.
Seek medical attention if pain worsens after 3 days, becomes severe or unrelenting, or occurs with redness, swelling, warmth, or discharge, as these may indicate infection or complications.
Redness & Inflammation

Redness and inflammation after hair transplant is localized erythema and inflammatory reaction appearing as visible redness with warmth, tenderness, and mild swelling around graft sites, affecting 22.4% of patients (16.33% mild, 5.14% moderate, 0.92% severe).
This reaction peaks 2-3 days post-surgery and subsides by 10-14 days in most patients, though fair-skinned individuals may experience erythema lasting 2-4 months, with complete resolution within weeks to months.
Redness and inflammation occur when mechanical trauma from graft extraction triggers inflammatory responses, potentially worsened by bacterial colonization. Risk factors include lighter skin types, large-session procedures, early post-operative washing, and folliculitis predisposition.
Treatment includes cool compresses, head elevation, topical or oral corticosteroids, and topical antibiotics for folliculitis. Seek medical attention if redness worsens, occurs with severe pain, discharge, fever, or persists beyond two weeks.
Learn More About Redness and InflammationTenderness

Tenderness after hair transplant is localized pain triggered by light pressure at donor or recipient sites without necessarily visible swelling, representing one of the most frequent complaints in the majority of patients within 48 hours post-surgery.
Tenderness is a temporary side effect, typically resolving within 1-3 days (average 2.3 days) and subsides completely without lasting effects, occurring when surgical disruption of blood vessels releases inflammatory substances that sensitize local pain receptors.
Treatment includes cold compresses, head elevation, and oral acetaminophen or NSAIDs as first-line therapy, with corticosteroids for refractory cases. Seek medical attention if tenderness worsens after 3-5 days or occurs with fever, discharge, or increasing redness to rule out infection.
Mild Bruising

Mild bruising from hair transplant procedures results from minor injury to the small blood vessels and the fluids used in the procedure, causing some blood to leak and gather in one area, leading to the bruising.
Bruising after a hair transplant is purely cosmetic and self-limiting, affecting approximately 20% of patients. Bruising appears 1-3 days post-surgery as faint to moderate bluish-purple discoloration around donor or recipient scalp sites (often extending to eyelids) with mild tenderness but no palpable swelling, and resolves spontaneously within 5-7 days.
To prevent bruising, maintain head elevation at 45° and apply firm headbands to reduce tissue oozing. Treatment for bruising consists of cold compresses for the first 48 hours, over-the-counter analgesics as needed, and natural resolution.
Seek medical help if bruising worsens after 5 days, becomes firm or fluctuant, involves severe pain, or shows infection signs.
Minor Bleeding
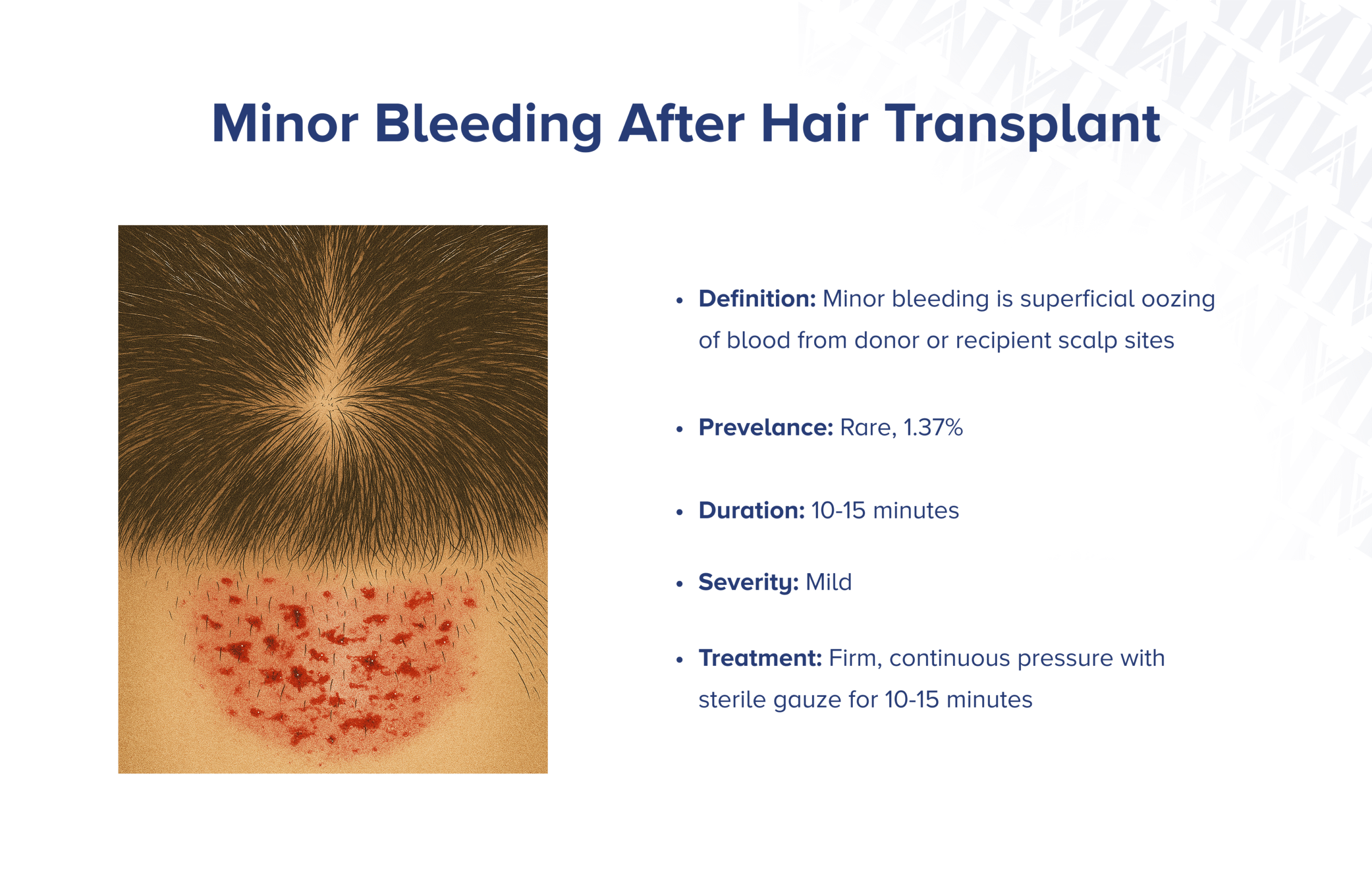
Minor bleeding from hair transplant procedures is superficial blood oozing from donor or recipient scalp sites caused by small blood vessel injury during graft harvesting or implantation, sometimes with graft displacement.
Bleeding after a hair transplant is generally mild and self-limited, rarely progressing to blood clots or graft loss when managed quickly. It typically stops within 10-15 minutes when firm, continuous pressure is applied and resolves completely without return once bleeding control is achieved. Bleeding after a hair transplant affects about 1.37% of patients.
Prevention involves stopping blood thinning medications before surgery, while treatment includes firm, continuous pressure with clean gauze for 10-15 minutes, supplemented with clotting agents or dilute epinephrine if needed.
Alert your doctor if bleeding continues beyond 15-30 minutes, returns despite adequate pressure, or occurs with growing swelling, severe pain, or blood clot signs.
Scabbing

Scabbing is the formation of hard crusts from dried blood, serum, and wound fluid over donor and recipient scalp areas, as part of normal healing after hair transplant. Scabbing affects 100% of patients, appearing as hard or rough crusts that are yellowish to brown in patches over graft sites and may be loosely or firmly attached to the scalp.
Scabbing forms immediately after surgery, persists for 3-7 days, and peels off naturally by day 7. Scabs lasting beyond 10 days indicate delayed healing. Scabbing completely disappears as the scalp heals, with crusts falling off naturally without affecting graft survival when handled properly.
To prevent scabbing, begin low-pressure saline spray and mild shampooing from days 2-3. Treat scabs with gentle saline or emollient massage from days 3-7, softening stubborn crusts with saline or dilute hydrogen peroxide.
See a doctor if scabs remain after 10-14 days, become painful, or occur with redness, swelling, or discharge to rule out infection.
Itching

Itching is a common discomfort in both donor and recipient scalp areas after hair transplant, affecting about 4.61% of patients. This localized sensation often occurs with scab formation during the healing process.
Itching usually starts around days 3-5 and resolves by the second week after hair transplant surgery with proper care. Itching is typically mild and self-limited, but severe scratching can dislodge grafts or break the skin, raising infection risk.
Treatment for itching involves saline or aloe vera-based sprays, gentle washing from day 3, and oral antihistamines or short-term topical corticosteroids if needed. See a doctor if itching persists beyond two weeks, becomes unusually severe, or occurs with redness, swelling, pain, or discharge.
Learn More About ItchingTemporary Numbness

Temporary numbness is a short-term loss of sensation in donor or recipient scalp areas after hair transplant, often caused by minor nerve injury during graft harvesting or implantation.
Temporary numbness occurs in 11% of hair transplant patients, presenting as reduced or altered sensation like tingling or hypersensitivity at donor or recipient sites. Temporary numbness usually resolves within 2-8 weeks, but can last up to 4 months in some cases. Permanent numbness is extremely rare.
Treatment for numbness starts with conservative management and observation; however, persistent neuropathic pain or neuroma formation may necessitate surgical exploration. See a doctor if numbness persists beyond 8 weeks, worsens, or occurs with pain or burning, suggesting neuroma formation.
Syncope
Syncope is a temporary loss of consciousness and muscle control caused by a short decrease in blood flow to the brain. It often happens as a vasovagal reaction, which can be triggered by anxiety or by anesthesia injections during hair transplant.
Syncope occurs in 0.24% of hair transplant patients (7 of 2,896 cases) and episodes go away within minutes when patients lie flat with their legs raised. Vasovagal episodes typically occur once and resolve without lasting issues.
See a doctor if you faint again, if it lasts over a few minutes, if you experience chest pain or a racing heart, or if you fall and hit your head.
Hiccups
Hiccups are involuntary spasms of the diaphragm and breathing muscles followed by sudden vocal cord closure, producing the characteristic "hic" sound. In hair transplant, hiccups result from irritation of the phrenic nerve during strip harvesting or FUE procedures.
Hiccups affect 0.2% of hair transplant patients. Most cases resolve within 48 hours without treatment. Treatment begins with simple techniques like breath-holding and bearing down, followed by medications like chlorpromazine if needed.
Seek medical attention if hiccups persist beyond 48 hours, prevent eating or drinking, or create severe distress requiring intervention.
What are the complications of hair transplant?
- Infection
- Folliculitis
- Skin Necrosis
- Wound Dehiscence
- Skin Discoloration
- Excessive Bleeding & Hematoma
- Extreme Scarring
- Cobblestoning
- Cyst Formation
- Keloid & Hypertrophic Scarring
- Pyogenic Granuloma
- Graft Failure
- Permanent Effluvium
- Nerve Injury
- Allergic Reaction
Infection

Infection is the invasion of pathogenic microorganisms into donor or recipient scalp wounds after hair transplant, leading to local inflammatory and purulent reactions. Infections are extremely rare, affecting less than 1% of hair transplant cases.
The condition usually appears 3 to 7 days after surgery and resolves within 1 to 2 weeks with proper treatment. While infections are typically mild and respond to antibiotics, untreated cases can lead to abscesses, graft loss, scarring, or rare instances of septicemia.
To prevent infections, carefully follow postoperative wound-care instructions. Treatment for infection after hair transplant may consist of antibiotics, drainage of abscesses, and moist dressings.
See a doctor if redness, swelling, pain, or discharge worsen after 7 days or if systemic signs like fever develop.
Folliculitis

Folliculitis is the inflammation or infection of hair follicles at donor or recipient sites after hair transplant, affecting 12.1% of patients. Folliculitis appears as small, tender, red papules or pustules around hair follicles, often with surrounding redness and mild itching.
Folliculitis usually clears up on its own within 7-10 days for superficial bacterial cases and heals without scarring if managed properly. Folliculitis can be treated by warm compresses and, for bacterial cases, 7-10 days of topical or oral antibiotics.
See a doctor if lesions persist beyond 7-10 days, spread, become increasingly painful, or occur with fever or deeper infection signs.
Skin Necrosis

Skin necrosis is the death of scalp skin tissue in donor or recipient areas after hair transplant. This rare condition affects 0.1% of hair transplant patients, though older reports noted up to 1.8% of cases.
The condition appears 3-7 days post-surgery, evolving into full-thickness necrosis within 1-2 weeks. Treatment of skin necrosis after hair transplant involves topical nitroglycerine, debridement, moist dressings, and surgical reconstruction for large defects.
See a doctor if persistent dusky or black skin, worsening pain, ulceration, or new skin loss develops beyond 7 days.
Wound Dehiscence
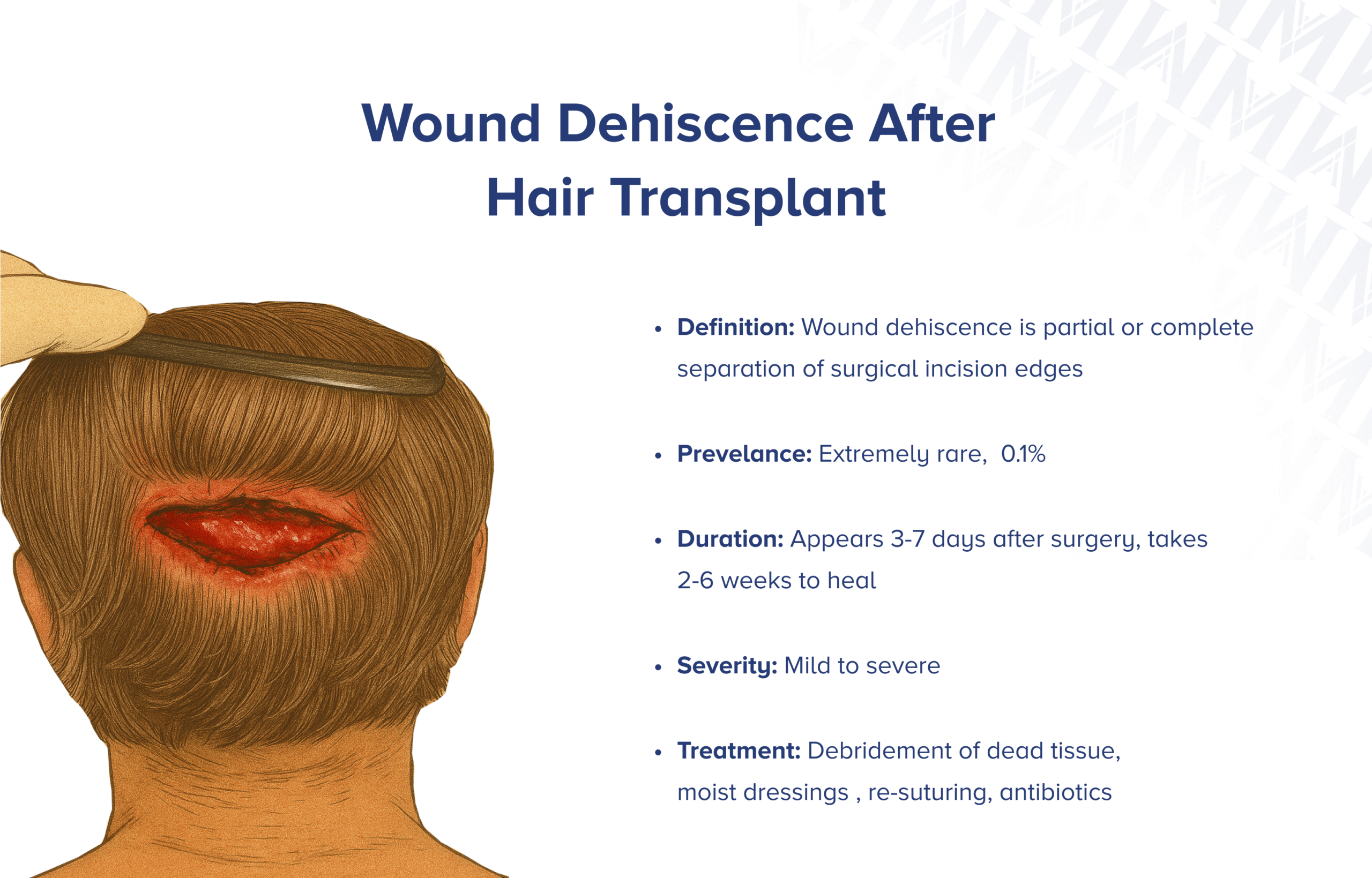
Wound dehiscence is the partial or complete separation of the surgical incision edges in the donor area after hair transplant. Wound dehiscence affects 0.10% of patients and occurs only with the FUT technique.
The condition develops within 3-7 days and heals over 2-6 weeks by secondary intention without re-closure. Wound dehiscence is treated with gentle debridement, moist dressings, and re-suturing for large defects.
Patients should see a doctor immediately if incision edges separate, with persistent discharge, increasing pain, or signs of infection, to arrange timely intervention.
Skin Discoloration

Skin discoloration (hyperpigmentation and hypopigmentation) is abnormal color changes with lighter or darker patches at donor or recipient scalp sites after hair transplant due to damage to pigment cells.
Discoloration appears in the first few weeks after surgery, with mild cases fading over 3-6 months and pronounced changes lasting up to 12 months. Treatment includes skin lightening treatments like hydroquinone and laser therapy.
See a doctor if color changes persist beyond 12 months or worsen.
Excessive Bleeding & Hematoma
Excessive bleeding and hematoma are complications where blood continues flowing from scalp sites despite standard measures or collects beneath the skin, forming tender swelling after hair transplant.
These complications occur in 1.37% of patients for excessive bleeding and under 1% for hematomas. Treatment involves firm direct pressure and medication injection for bleeding, and prompt surgical drainage with compression bandages for hematomas.
Seek immediate medical attention if bleeding continues beyond 15-20 minutes or hematomas rapidly expand.
Keloid and Hypertrophic Scarring

Keloid and hypertrophic scarring are abnormal raised scars from exaggerated wound healing after hair transplant. Donor-site thick scarring after FUT hair transplant affects 15.1% of patients, while true keloids occur in less than 1%.
Treatment involves steroid injections, often combined with silicone sheets. Stubborn cases benefit from freezing therapy, laser, surgical removal, or special medication injections.
See a doctor if scars remain raised, symptomatic, continue enlarging, or cause appearance or movement concerns.
Cobblestoning
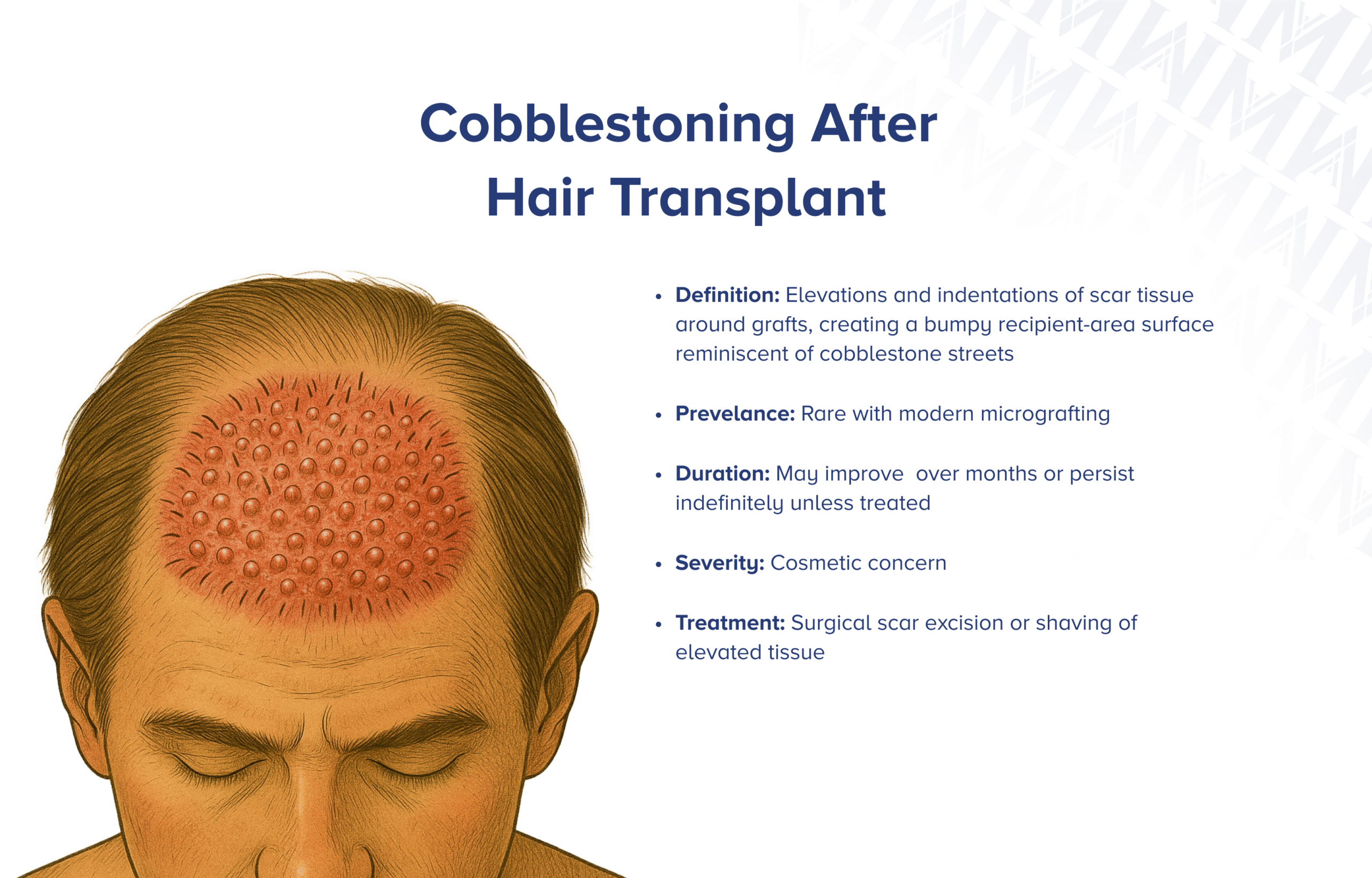
Cobblestoning is characterized by raised areas and depressions around grafts, creating a bumpy scalp surface. Cobblestoning was more common with older punch-graft techniques and is rare with modern small grafts.
Treatment involves observation, application of tissue glues immediately after surgery, and, for persistent cases, surgical scar removal or shaving of elevated tissue.
See a specialist if uneven graft sites remain noticeable beyond 6-12 months to discuss correction options.
Cyst Formation

Cyst formation after hair transplant involves the development of epidermal inclusion or subdermal cysts at donor or recipient sites, presenting as firm, skin-colored nodules. The exact incidence is unclear, but it is rare.
Treatment for cysts typically involves incision and drainage or complete excision, along with warm compresses and antibiotics if infected.
Medical evaluation is necessary if they grow, become painful or red, or show signs of infection like discharge or fever.
Pyogenic Granuloma

Pyogenic granuloma is a benign overgrowth of capillary blood vessels and granulation tissue that can occur at hair-transplant sites. In a study of 533 hair-transplant procedures, it occurred in 0.2% of patients.
Treatment for pyogenic granuloma typically involves complete surgical excision through curettage and cautery, with options like laser ablation, cryotherapy, or topical agents such as timolol or imiquimod as alternatives.
Medical evaluation is necessary for any new, rapidly growing red nodules at transplant sites, especially if they bleed easily or cause discomfort.
Graft Failure
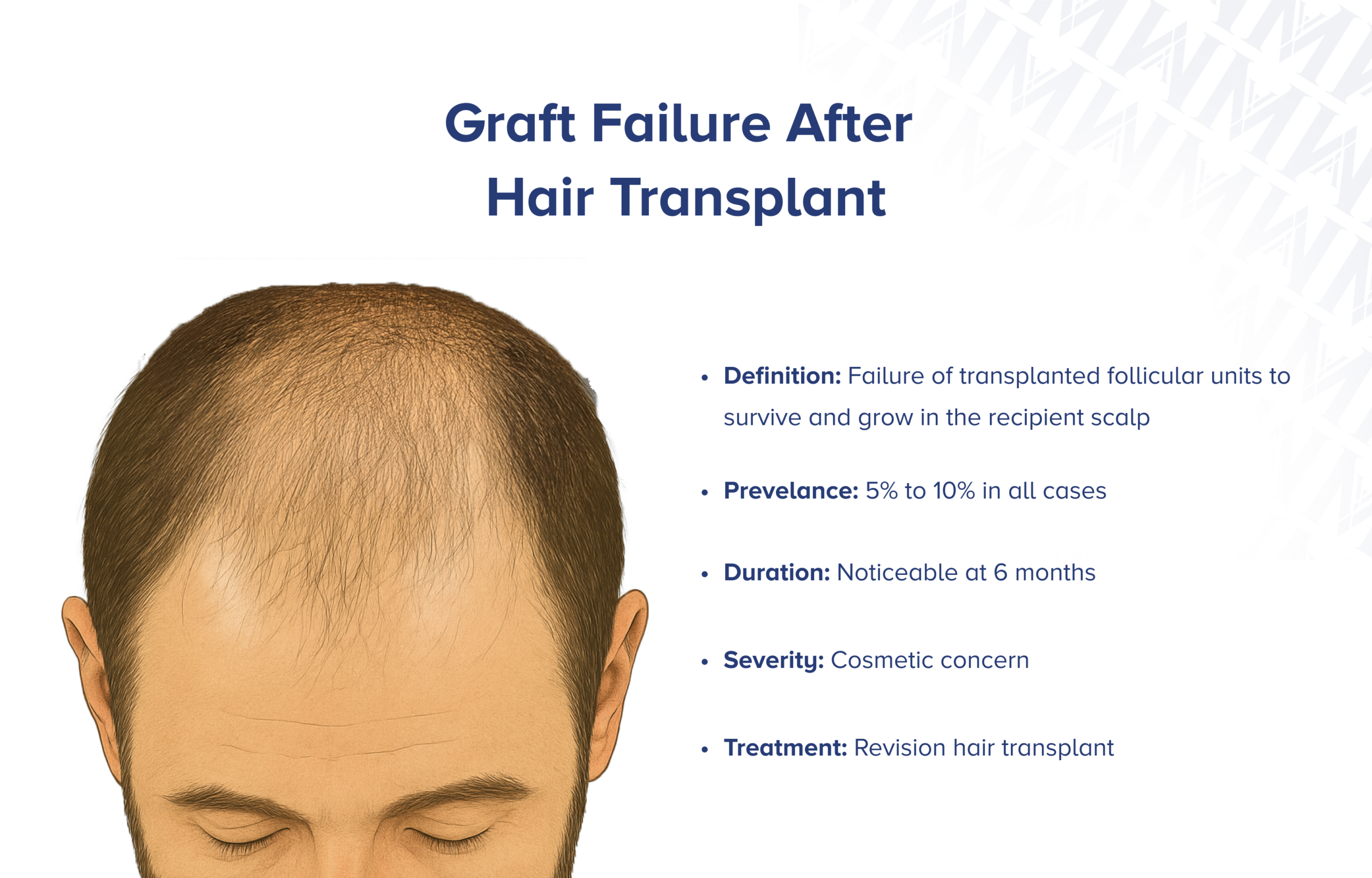
Graft failure occurs when transplanted follicular units do not survive in the recipient scalp, leading to hair absence in the transplant area. Most modern FUE series report over 90% follicle survival at 12 months, indicating a 5-10% graft failure rate.
Graft failure can be treated with a second revision hair transplant. Consult your surgeon if little to no hair growth is observed by 6-9 months post-op or if early signs of graft necrosis appear within the first few weeks.
Permanent Effluvium

Permanent effluvium is irreversible hair loss from hair transplant, resulting from the destruction of hair follicles and the formation of scar tissue. This condition is extremely rare, occurring in less than 0.1% of cases.
Treatment and prognosis focus on cosmetic rehabilitation, including scar excision or follicular unit transplant into stable scar tissue, micropigmentation, or hairpieces.
Consult a doctor if there is no hair regrowth in the transplanted area by 9-12 months or if signs of scalp necrosis or progressive scarring develop.
Nerve Injury
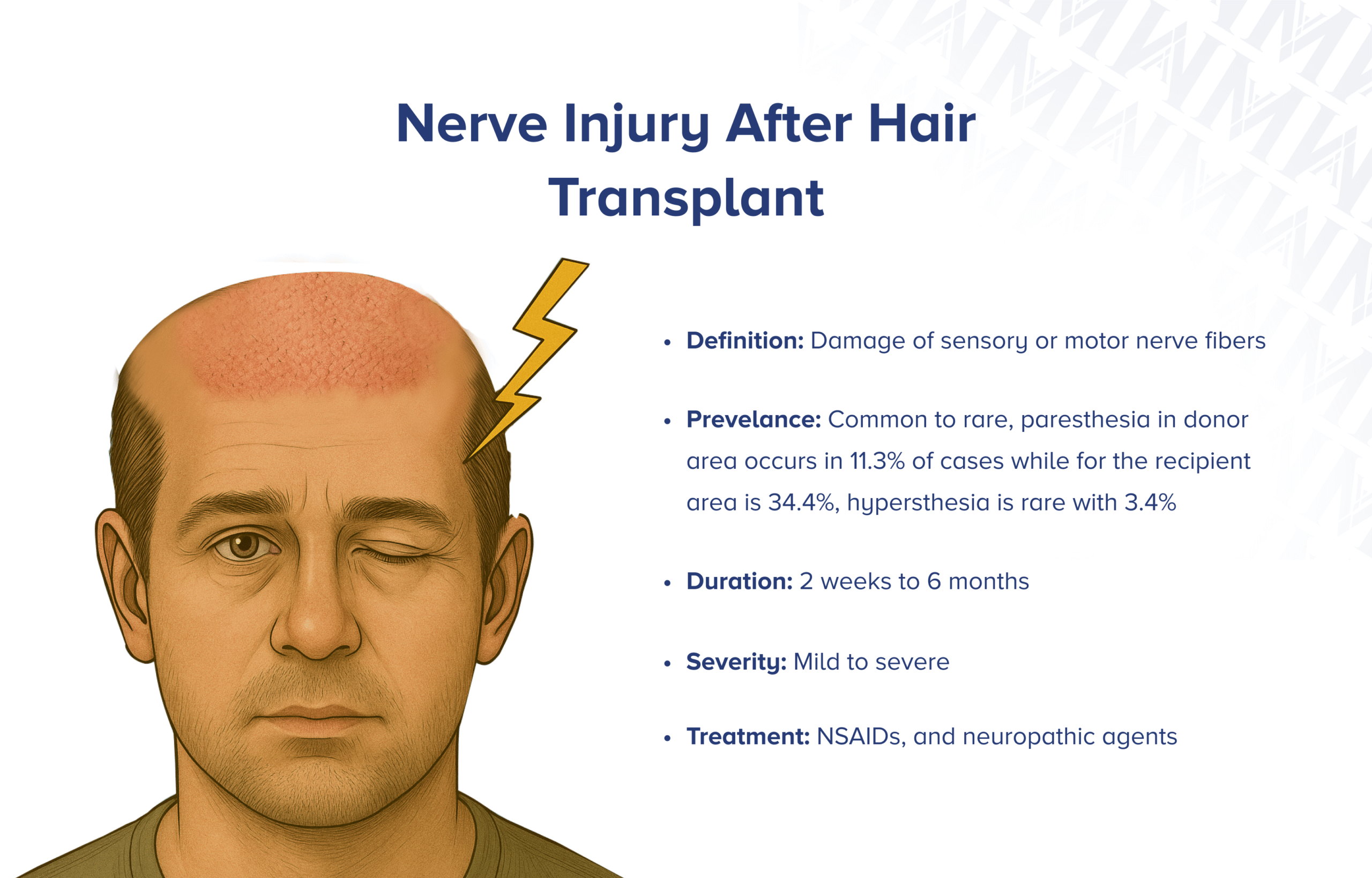
Nerve injuries are temporary sensory disturbances and mild motor weakness in facial muscles due to minor nerve trauma during hair transplant. Nerve injuries affect less than 0.1% of patients.
The condition typically resolves within a few weeks to 1-3 months, though some cases may take up to 6 months. Treatment focuses on supportive management, NSAIDs for discomfort, and neuropathic agents like gabapentin for pain.
See a doctor if symptoms persist beyond three months, worsen, or occur with severe pain, significant asymmetry, or functional impairment.
Allergic Reaction

An allergic reaction after hair transplant occurs when the immune system reacts to medication used during the procedure. True allergic reactions are extremely rare, occurring in well under 1% of cases.
First-line treatment for mild reactions includes antihistamines and corticosteroids, while intramuscular epinephrine is crucial for anaphylaxis, along with airway support and IV fluids.
Immediate medical attention is essential for respiratory difficulty, facial or throat swelling, hypotension, or worsening skin reactions that do not improve within 24 hours.
What are the risks of hair transplant?
- Poor Aftercare
- Insufficient Donor Supply
- Multiple Sessions
- Overharvesting
- Unnatural Appearance
- Color Mismatch
- Progressive Hair Loss
Poor Aftercare
Poor aftercare includes failing to follow postoperative protocols like wound cleansing, head positioning, medication schedules, and activity restrictions after hair transplants. Studies show medication nonadherence rates of up to 50%.
Inadequate aftercare increases the risk of infection, graft loss, and unsightly scarring, affecting safety and cosmetic results. Patients should contact their surgeon if they have questions about care or notice warning signs.
Insufficient Donor Supply

Insufficient donor supply occurs when the safe donor zone lacks enough healthy follicular units for a successful hair transplant. In advanced androgenetic alopecia (Norwood V and above), donor hair often falls short.
Limited donor reserve affects density and coverage, resulting in suboptimal cosmetic outcomes. The donor supply must be analyzed prior to surgery to ensure the best results.
Multiple Sessions

Multiple sessions refer to needing more than one hair transplant to achieve the desired density or coverage. In one large FUE study, 14.8% of patients underwent two or more surgical sessions.
Multiple sessions can lead to higher costs, increased downtime, and potential challenges for future procedures. Patients should follow up with their surgeon 6-12 months later if further sessions are needed.
Overharvesting

Overharvesting occurs when excessive follicular units are extracted during a hair transplant, resulting in permanent donor scalp damage. Overharvesting and technical errors are common risks in FUE hair transplants.
Treatment options include revision hair transplants and non-surgical options like scalp micropigmentation. A specialist evaluation is advised if thinning or scarring persists beyond 6-12 months.
Unnatural Appearance

Unnatural appearance in hair transplant arises from poorly designed hairlines, pluggy grafts, or incorrect angulation. Unnatural appearance is one of the most frequent aesthetic complaints after hair transplant.
Options include revision transplants for better density and angle, scalp micropigmentation, or graft removal. Consult a hair-restoration specialist if you're dissatisfied with the transplant's appearance 6-12 months post-op.
Color Mismatch

Color mismatch occurs when there is a difference in hue or shade between transplanted hairs and surrounding scalp hair. This occurs when non-scalp hair, such as beard or body hair, is used.
Color mismatch in hair transplant can be addressed with hair-coloring products, scalp micropigmentation, or additional grafting. If color mismatch causes distress, consulting a hair transplant surgeon or dermatologist is advisable.
Progressive Hair Loss

Progressive hair loss after hair transplant happens when native hair continues to miniaturize due to ongoing androgenetic alopecia. Most hair transplant patients face this issue as the genetic balding process persists despite surgery.
Post-transplant care includes topical minoxidil and oral finasteride to slow native hair loss, with potential for additional transplant sessions as balding continues. Patients should discuss hair loss progression and maintenance therapy with their surgeon.
Hair transplant side effects by hair transplant technique
Hair transplant methods share many common post-op effects, but certain issues tend to be more pronounced with each approach:
| FUE Hair Transplant Side Effects | DHI Hair Transplant Side Effects | FUT Hair Transplant Side Effects |
|---|---|---|
| Temporary Numbness | Tenderness | Pain & Discomfort |
| Skin Discoloration | Minor Bleeding | Tenderness |
| Overharvesting | Hiccups | |
| Multiple Sessions | Temporary Numbness | |
| Wound Dehiscence | ||
| Keloid & Hypertrophic Scarring |
Short term vs long term side effects complications, and risks
Below is an overview categorizing the short term versus long term outcomes you may experience following a hair transplant procedure.
| Short Term | Long Term |
|---|---|
| Short Term Side Effects • Swelling • Scabbing • Pain & Discomfort • Redness & Inflammation • Tenderness • Mild Bruising • Minor Bleeding • Itching • Syncope • Hiccups |
Long Term Side Effects • Shock Loss • Temporary Numbness |
| Short Term Complications • Infection • Folliculitis • Excessive Bleeding & Hematoma • Wound Dehiscence • Allergic Reaction |
Long Term Complications • Skin Necrosis • Skin Discoloration • Keloid & Hypertrophic Scarring • Cobblestoning • Cyst Formation • Pyogenic Granuloma • Graft Failure • Permanent Effluvium • Nerve Injury |
| Short Term Risks • Poor Aftercare |
Long Term Risks • Insufficient Donor Supply • Multiple Sessions • Overharvesting • Unnatural Appearance • Color Mismatch • Progressive Hair Loss |
Hair Transplant Side Effects by Demographics
Age significantly influences both recovery and complication risks after hair transplant. Patients between the ages of 18 and 50 have no significantly higher risk of developing a certain side effect or complication. Patients over 50 often face slower wound healing due to age-related declines in blood flow and cell regeneration.
Hair Transplant Side Effects in Women
Although patients of all genders can experience any hair transplant side effect or complication, women are more likely to experience "shock loss," according to the ISHRS.
Hair Transplant Side Effects by Hair Type
Straight hair tends to look less dense after transplant unless a high graft count is used. Wavy hair patients often notice frizzy, unruly regrowth in the first few months. Curly hair carries a small chance of "post-transplant curly hair." Kinky or coily hair has the highest risk of graft damage and elevated risk of keloid scarring.
Hair Transplant Side Effects by Skin Type
Darker skin (Fitzpatrick IV-VI) carries a significantly higher risk of keloid and hypertrophic scarring. Very fair skin (Fitzpatrick I-II) is more prone to pronounced redness and visible scabbing. Thin or soft scalp increases risk for scalp necrosis, while thick or firm scalp tissue often requires increased force, leading to higher graft damage rates.
Conclusion
Hair transplant procedures, though highly effective and increasingly refined, come with a range of possible side effects, complications, and long-term risks. Most patients experience only mild, temporary reactions that resolve with proper care, but rare medical complications and aesthetic concerns can still occur, especially with poor surgical technique or inadequate aftercare.
By understanding these outcomes in advance and working with experienced professionals, patients can greatly improve their chances of a safe recovery and satisfying results. The key to success lies in proper planning, selecting qualified surgeons, following aftercare instructions meticulously, and maintaining realistic expectations throughout the journey.
Key Takeaways
- Most side effects are temporary and resolve within 1-2 weeks
- Serious complications occur in less than 5% of patients
- Proper aftercare is crucial for optimal results and complication prevention
- Understanding risk factors helps patients make informed decisions
- Early recognition and treatment of complications leads to better outcomes
- Choose experienced surgeons and accredited facilities for best results

